best office chair for sacroiliac problems

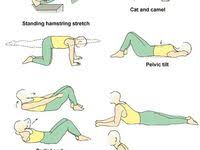
The first 10 days are considered the acute phase. If symptoms do not resolve, days 10-180 are considered the subacute phase. Pain lasting longer than 6 months is considered the chronic phase. Physical therapy focuses on pain control in the acute phase. Modalities such as ultrasonography with or without phonophoresis, deep and superficial heat, and superficial cold treatments can reduce pain. Neural therapies such as deep tissue massage, myofascial release, and muscle energy stretching techniques can also help. Pelvic myofascial stretching in the neutral spine position can be used for immediate, short-term relief of discomfort. By identifying activities that aggravate the condition, the physician or therapist can have the patient avoid these activities. Although in the acute-phase muscle spasms may prevent frank manipulation, less aggressive techniques such as muscle energy stretching can be very helpful. Patients may experience difficulty or even worsening symptoms with physical therapy treatments in certain cases.
In these patients, reevaluate the diagnosis and consider other diagnostic possibilities (eg, infection, inflammatory disease, malignancy, neural [lumbosacral root] injury). Patients with acute inflammatory disorders or infections should not usually be administered heat treatments. Patients who cannot perform physical therapy may also have a functional component to their disorder or an underlying psychologic disorder, which needs to be addressed. Often, oral medications can be quite effective in the acute phase. Nonsteroidal anti-inflammatory drugs (NSAIDs) are used judiciously in this phase, often with good results. In the first 24-72 hours, a muscle relaxant can be quite effective if a myofascial component to the pain is present. Ice can be considered in the first 48-72 hours; then, the typical switch to heat or contrast treatments is warranted. Oral medication management may change if the pain persists into the subacute and especially the chronic phase. Chronic lower back pain from any source often leads to the development of a cognitive/behavioral component.

In such cases, the use of antidepressants, anticonvulsants, and antiarrhythmic topical and oral medications has been reported to benefit certain selected patients. Because the potential benefits of any of these medications is uncertain, their use must be balanced against their potential adverse effects. Surgical intervention is rarely used for nontraumatic SIJ pain.Surgery is considered only in patients with chronic pain that has lasted for years, has not been effectively treated by other means, and has led to an extremely poor quality of life; the procedure is a fusion across the joint. A randomized, controlled trial by Polly et al found that patients who underwent minimally invasive SIJ fusion with triangular titanium implants achieved greater pain and disability relief at 24-month follow-up than did those who underwent nonsurgical management. The rates of pain and disability improvement for the fusion patients (102 subjects) at 24 months were 82.0% and 65.9%, respectively, compared with less than 10% for both pain and disability in the nonsurgical patients (46 subjects).

Similarly, a randomized, controlled study by Sturesson et al also found better alleviation of pain and disability with SIJ joint fusion with triangular titanium implants than with conservative management. In the fusion patients (52 subjects), the mean lower back pain score had improved by 43.3 points at 6 months, compared with 5.7 points in the conservative treatment group, while the mean disability score had improved by 26 points in the fusion patients, compared with 6 points in the conservative management group.
cheap graco high chairs A study reported that ilio-sacral screws can be safely used to treat sacral fractures and sacroiliac joint injuries in children.
power chair motor brushes Consultation with a rheumatologist is necessary when the possibility of an underlying inflammatory disorder exists.
green office chair staples
Consultation with a musculoskeletal specialist is often helpful. The musculoskeletal specialist should provide each patient with a functional assessment, can direct nonoperative treatment, and can communicate with the entire treatment team (eg, physical therapists, trainers). Often, a physiatrist (specialist in the field of physical medicine and rehabilitation) can provide a unique, functional-based history and examination that can lead to an accurate diagnosis and a holistic treatment program. In the immediate acute phase, treatment consists of pain reduction through pain medications, rest, and avoidance of the inciting activity. Anti-inflammatory treatment with NSAID medications and externally applied ice is often helpful. Recommend the patient return to usual activities as soon as possible, usually within 24-48 hours. Sometimes a local trigger point injection into the muscle can relieve symptoms. [22, 23, 24, 25] If the pain does not resolve well in the first 2-3 weeks, an intra-articular injection under fluoroscopic guidance should be considered.

SIJ injection is frequently performed with a mixture of anesthetic and steroid, as described by Fortin in 1994 and others. [8, 26, 27, 28, 29] When the actual source of the patient’s discomfort is unclear, postinjection pain reduction offers significant diagnostic information. Fluoroscopic guidance is important because, although a local blind injection into the area of maximal pain can be temporarily effective, the needle rarely enters the joint. CT scanning or MRI can also be used to guide injections into the SIJ, with excellent reliability. Günaydin and colleagues reported that 20 of 31 patients with spondylarthropathy reported subjective improvement after the first SIJ injection of MRI-guided corticosteroid, and 9 of 15 patients reported subjective improvement after the second injection. [28] The improvement lasted for a mean of 8.7 for the first group and 16.1 months for the second group. Luukkainen and colleagues reported that periarticular injection of methylprednisolone may be effective in the treatment of pain in the region of the SIJ in nonspondyloarthropathy patients from a study of 24 consecutive patients.
Although these studies are promising, they are not randomized, placebo-controlled studies. Therefore, before efficacy can be established, randomized, placebo-controlled studies must be undertaken. Even if the injections do relieve the patient's pain, the relief from the injections alone is very often short-lived. Therefore, using the injections only as part of an interdisciplinary rehabilitation program is important. The pain relief offers a window of opportunity to increase the rehabilitation. The point in the course of recovery when a second or even third injection should be attempted is unclear. Most clinicians wait 2-4 weeks before proceeding with a repeat injection. Manipulation has been reported in multiple studies as effective treatment for acute lower back pain. However, studies specifically on SIJ syndrome are less abundant. The SIJ is accessible to manipulation treatments and these may be extremely effective. As with other passive modalities, these treatments should be coupled with an extensive active rehabilitative program.

Manipulation following intra-articular injection has been reported anecdotally to be beneficial in selected cases. In chronic conditions, some practitioners believe that SIJ pain is due to hypermobility of the joint, which occurs because of laxity in the ligamentous complex. Prolotherapy is a series of saline and glucose injections applied to the SIJ ligaments to cause an inflammatory reaction, which results in scarring and tightening of the ligaments and a reduction in pain. However, no satisfactory outcome investigations have been performed on prolotherapy for this condition. A relatively more recent procedure, radiofrequency denervation, has been advocated for the treatment of especially recalcitrant sacroiliac dysfunction.The procedure was thought to be ineffective for SIJ pain because the innervation to the joint is so diffuse. However, in a study by Gevargez and colleagues, the authors reported that 3 months after the procedure, 13 patients (34.2%) were completely free of pain.